Vasectomy
A vasectomy is a minor surgical procedure performed to block sperm from leaving the body. It’s a highly effective and common birth control option. Experts estimate that one in five men over age 35 in the United States has had a vasectomy. It’s a simple procedure, and it doesn’t take long for most men to recover. As minimally invasive urologic procedures go, vasectomies are inexpensive, even as an out-of-pocket charge, and especially if you have health insurance that covers it.
You will, of course, want to consider your decision to have a vasectomy carefully. It’s possible – and not uncommon – to reverse a vasectomy, but a reversal procedure is generally more invasive and more expensive than a simple vasectomy. The success rate of a reversal depends on many factors. That said, there are ways to retrieve sperm cells from the testes for in vitro fertilization, so if a vasectomy reversal is not successful, there may still be options for starting a family.
If you aren’t sure a vasectomy is right for you, there are a number of other contraception options to consider.

Vasectomy: How Does It Work?
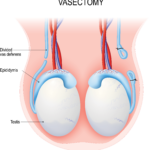
To review the essentials of male reproductive anatomy, sperm cells are made by your two testes (testicles). Attached to each testis is a coiled area called the epididymis. Once the sperm cells are created, they move to the epididymis where they mature. They’re stored in the epididymis for up to 6 weeks until they’re ejaculated.
When sexual stimulation starts, sperm cells move from the epididymis to the vas deferens (sometimes just called the “vas”), a tube that connects the epididymis to the urethra. Sperm cells can be stored in the vas as well. In fact, it’s common for some sperm cells to overflow into the vas before ejaculation. Sperm cells that aren’t ejaculated can stay behind in the vas, too.
Along the way, seminal fluid and sperm cells mix to form semen, which is expelled through the urethra out the tip of your penis when you ejaculate.
During a vasectomy, the vas is cut, so the sperm cells can’t make it to the urethra. (You have two vas deferentia – one vas for each testicle. In a vasectomy, both tubes are cut.)
After a vasectomy, your testes will continue to make sperm, but your body will simply absorb them. You’ll still ejaculate semen, but the fluid won’t contain sperm (once sperm has cleared from your system, which takes roughly three months). Your orgasms won’t feel any different. There is a minimal loss in semen volume.
Vasectomy Advantages
It takes time for a vasectomy to fully take effect. But once it does, the success rate for pregnancy prevention is around 99.95%. Sex can be more spontaneous, and for some, sex is more pleasurable without the worry of an unplanned pregnancy.
Vasectomy Disadvantages
As already mentioned, a vasectomy isn’t effective immediately. You’ll need to use another form of birth control until your semen is clear of sperm.
Also, while a vasectomy is estimated to be 99.95% effective, there is still a less than 1% chance that pregnancy may occur. And it does happen. Only abstinence is 100% effective for any type of birth control.
Safe sex is still critical after a vasectomy, too. Vasectomy does not provide any protection against sexually-transmitted infections (STIs). You’ll still need to use condoms or dental dams every time you have sex unless you know your partners do not have STIs.
What to Expect
Before your vasectomy
We’ll schedule an informational visit to explain the procedure. This is a good time to ask questions. Consider writing down your questions beforehand. Your partner is welcome to join you and ask questions too.
In the week or so before your vasectomy, it’s important not to take any nonsteroidal anti-inflammatory drugs (NSAIDs), like aspirin or ibuprofen. These medications can thin your blood and put you at higher risk for bleeding. If you’re not sure about a specific drug, just give our office a call.
As with most minor medical procedures, you should also have someone drive you to and from your vasectomy appointment.
The vasectomy itself
Vasectomy is actually a straightforward procedure, and it usually takes about a half hour. Vasectomies are typically performed in our office. A local anesthetic is used. If you’re feeling especially anxious, you may choose to be sedated. In some cases, general anesthesia may be used.
After your scrotum is shaved and washed, the local anesthesia will numb the vas deferens area. Your surgeon will locate the vas deferens, which will be accessed in one of two ways:
- Conventional vasectomy. With this type of procedure, your surgeon will access your vas deferens through 1 or 2 small incisions in your scrotum.
- No-scalpel vasectomy. The vas deferens will be accessed through a small puncture in your scrotum. The puncture is made with forceps that stretch the skin.
At this point, a small section of your vas deferens will be cut and, in some cases, removed. Next, your surgeon will clip, tie, or cauterize (seal with heat) the ends of the remaining vas segments. This blocks the sperm’s travel path. You might feel a pulling sensation.
The procedure is then repeated for your other vas.
If you’re having a conventional vasectomy, the incisions will be closed with sutures. If it’s a no-scalpel procedure, you shouldn’t need sutures.
You should be able to go home shortly after the procedure is finished. As noted earlier, plan to have someone bring you home.
Potential complications
According to the American Urological Association (AUA), about 1% to 2% of men undergoing vasectomy experience surgical complications, such as hematoma (where blood collects outside a blood vessel).
Recovery
When you get home
We’ll give you detailed instructions to follow while you recuperate.
The most important element of a successful recovery is rest. Be prepared to limit your activities for five days to a week, especially lifting heavy things. Wearing a jockstrap might make you more comfortable. Don’t bathe or swim for up to two days.
You might be able to return to work in a few days, depending on how you’re feeling. But you might have to modify some of your work activities for a short time. That will be part of our follow up discussion.
Placing an ice pack on the affected area (over your clothing) can help reduce pain and swelling. You might also try taking some Tylenol (acetaminophen), but we recommend that you avoid aspirin or ibuprofen, as these drugs can raise the risk of bleeding or bruising. We can prescribe a stronger medication if you need it.
What to watch for
Most men go through vasectomy without any serious complications. But you should be on the lookout for bleeding, swelling, fever, redness, and signs of infection. Give us a call if you experience these symptoms.
Some men develop a mass called a sperm granuloma after vasectomy. This forms as part of your immune system’s response to stray sperm cells coming from the cut vas deferens. It’s usually nothing to worry about and should go away on its own, but it can be uncomfortable. In severe cases, it may need to be surgically removed.
Post-vasectomy pain syndrome
Some men develop significant chronic pain in their testicles or scrotum after a vasectomy, although this is not common. Usually, this pain can be treated with medications and warm baths. If it becomes severe, we might have you see a pain specialist. Surgery or vasectomy reversal might be considered at some point.
What about sex?
After your vasectomy, you’ll also need to avoid ejaculation for about a week. And for the next 16 to 18 weeks, you’ll still need to use birth control.
Why? Remember, each vas deferens is connected to the epididymis, a storage area for sperm cells. And sperm cells can be stored in the vas as well. When the vas is cut, there can still be residual sperm cells lingering, and these cells can still mix with semen when you ejaculate. So, until these remaining sperm cells clear, you will still be able to get a partner pregnant.
We’ll be monitoring the situation, though. During your follow-up appointments, we’ll do a semen analysis to check how much sperm is left in your semen. Once we’ve determined all the sperm have cleared, your vasectomy should be effective.
For most men, it takes about three months – or 20 ejaculations – for sperm to clear. But every man is different, and it might take more or less time. It’s important to keep all of your follow up appointments.
Aside from the need to use birth control until your semen clears, you shouldn’t see any major changes in your sex life. You’ll still ejaculate semen like you did before, but once cleared, the semen won’t contain any sperm. (Sperm makes up about 5% of semen, so the volume you ejaculate shouldn’t change significantly.) You’ll still feel the same pleasure from orgasm. Your partner won’t be able to tell you’ve had a vasectomy.
Your body will still produce sperm cells, but they’ll simply be absorbed by the body.
Vasectomy reversal
Oftentimes life circumstances change. You might at some point consider a vasectomy reversal (vasovasostomy).
As noted earlier, the reversal procedure is more complex than the vasectomy itself. It may also be more expensive, and it’s not always covered by insurance.
The success rate of a reversal depends on several factors and can vary widely. The more years that have passed between your vasectomy and your reversal procedure, in particular, is a determinant of whether a vasectomy reversal will be successful.
But an unsuccessful vasectomy reversal doesn’t mean there aren’t viable sperm cells available. For some men, sperm cells can be surgically retrieved from the testes.
It used to be commonly believed that over time, sperm antibodies damaged all the sperm in a man’s body. We now know how to find and identify healthy sperm, even in men who had vasectomies many years ago. The retrieved sperm can be used for IVF (in vitro fertilization) procedures.
Also, some men decide to freeze their sperm before a vasectomy, just in case they change their minds later.
Resources
American Urological Association
“Vasectomy: AUA Guideline”
(Approved by AUA Board of Directors in May 2012. Amended in 2015)
Johns Hopkins Medicine
“Overview of the Male Anatomy”
https://www.hopkinsmedicine.org/health/wellness-and-prevention/overview-of-the-male-anatomy
Medical News Today
Villines, Zawn
“What to know about sperm production”
(July 31, 2019)
https://www.medicalnewstoday.com/articles/325906
MedlinePlus
“Sperm release pathway”
(Reviewed: January 15, 2020)
https://medlineplus.gov/ency/anatomyvideos/000121.htm
UpToDate.com
Viera, Anthony J., MD, MPH
“Patient education: Vasectomy (Beyond the Basics)”
(Topic last updated: June 12, 2019)
https://www.uptodate.com/contents/vasectomy-beyond-the-basics
Urology Care Foundation
“What is a vasectomy?”
https://www.urologyhealth.org/urologic-conditions/vasectomy
“What is sperm retrieval?”
https://www.urologyhealth.org/urologic-conditions/sperm-retrieval
Verywellhealth.com
Boskey, Elizabeth, PhD
“The Anatomy of the Epididymis”
(Reviewed: September 1, 2020)
https://www.verywellhealth.com/epididymis-anatomy-4774615
Hayes, Kristin, RN
“The Anatomy of the Vas Deferens”
(Reviewed: July 9, 2020)
https://www.verywellhealth.com/vas-deferens-4846228